Perimenopause & Menopause Glossary
The Opal & Joy perimenopause and menopause glossary is your trusted, science-based guide to understanding the language of hormonal change. This cohesive resource clearly explains key perimenopause and menopause terms, so you can feel informed, confident, and in control of your health.
From estrogen dominance to brain fog, HRT, and restorative sleep, every definition is written by wellness experts and fact-checked against leading medical sources.
Whether you’re curious about symptoms, testing, or treatment options, you’ll find everything you need to understand perimenopause and menopause clearly, compassionately, and confidently.
Glossary of Menopause & Perimenopause Terms
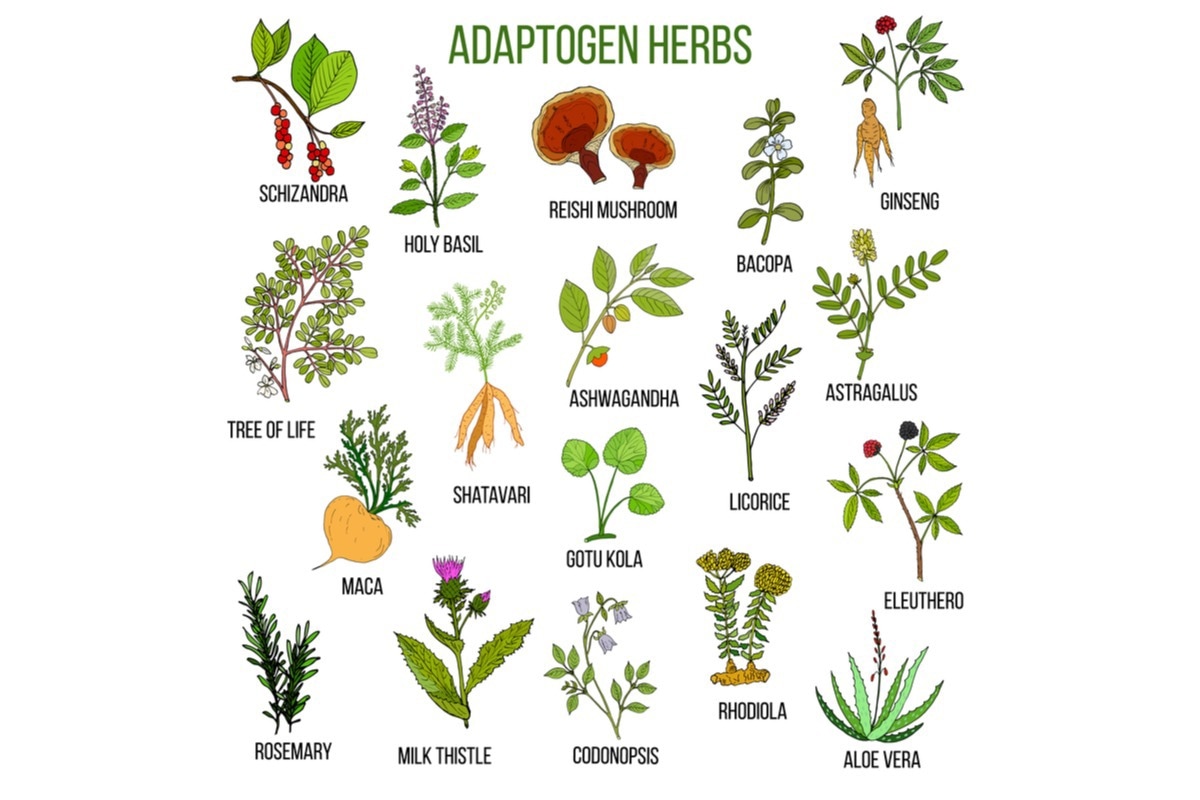
Adaptogens
Adaptogens are a group of herbs traditionally used to support the body’s response to stress. They are thought to help with resilience to physical and emotional stressors, although scientific evidence varies by herb. Some women explore adaptogens during perimenopause to support calm and energy, especially when stress feels elevated. Discuss use with a clinician, as adaptogens can interact with medications.
Androgen Decline
Androgens are hormones, including testosterone and dehydroepiandrosterone (DHEA), that contribute to libido, energy, muscle mass, and mood. In women, androgen levels decline gradually with age. This decline can contribute to reduced sexual desire and changes in body composition during midlife.
Anti-Müllerian Hormone (AMH)
Anti-Müllerian hormone is produced by ovarian follicles and reflects the remaining egg supply. AMH decreases as egg quantity and quality decline with age. While AMH testing estimates ovarian reserve, it does not accurately predict the onset of menopause.
Anovulatory Cycles
Anovulatory cycles are menstrual cycles in which ovulation does not occur. Without ovulation, the hormone progesterone is not released in the typical pattern. These cycles become more common in perimenopause and can cause irregular, missed, or heavy periods.
Bioidentical Hormones
Bioidentical hormones have the same molecular structure as hormones naturally produced by the human body. Some FDA-approved hormone therapies are bioidentical; custom-compounded products are not standardized and can vary in dose and purity. Discuss risks and benefits with a clinician.
Bone Density
Bone density refers to the amount of mineral in bone tissue. Strong bones have higher density. Estrogen helps maintain bone density; as estrogen declines after menopause, bone breakdown can outpace rebuild, leading to reduced density and higher fracture risk.
Brain Fog / Cognitive Changes
Brain fog is a common term used to describe changes in memory, concentration, word-finding, and mental clarity. During perimenopause, fluctuating estrogen levels affect neurotransmitters involved in attention and verbal recall. Sleep disruption, stress, and anxiety can further worsen cognitive sharpness. Brain fog is usually temporary, but persistent symptoms should be discussed with a healthcare provider to rule out other causes.
Breast density
Breast Density describes the proportion of fibrous and glandular tissue compared to fatty tissue in the breast. Dense breasts are more common in younger women but can persist into midlife. Higher density can make mammograms harder to interpret and is itself a modest risk factor for breast cancer.
Cardiovascular Disease Risk
Cardiovascular disease includes heart attacks, strokes, and other conditions of the heart and blood vessels. After menopause, lower estrogen levels are associated with changes in cholesterol, blood pressure, and vessel elasticity that increase long-term heart disease risk. Regular screening and healthy lifestyle habits help protect cardiac health.
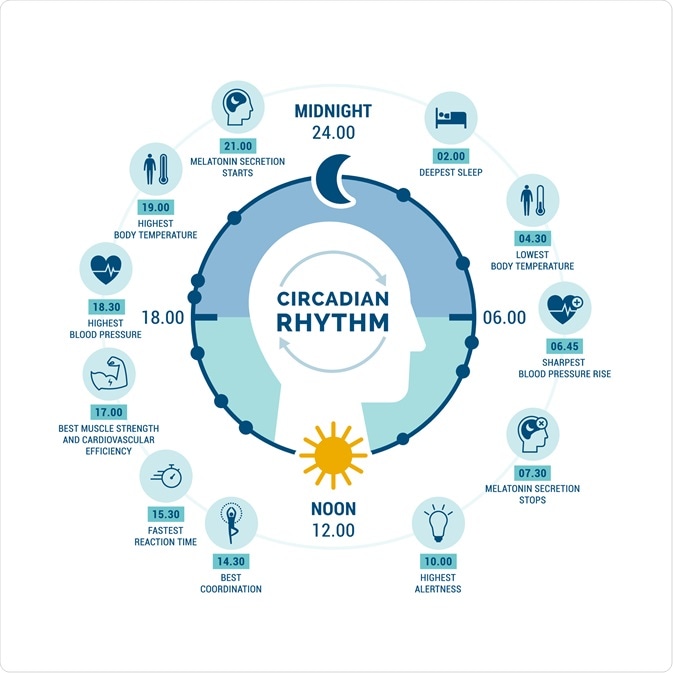
Circadian Rhythm
Circadian rhythm is the body’s internal 24-hour clock that governs sleep-wake cycles, hormone release, body temperature, and metabolism. It is strongly influenced by light exposure and daily routines. Disruption during perimenopause can worsen sleep quality and daytime energy.
Climacteric
Climacteric refers to the years of reproductive decline and transition during perimenopause and menopause. It is used mainly in clinical and research contexts to describe the entire span of physiological change, not just symptom clusters.
Contraception in Perimenopause
Although fertility declines in perimenopause, pregnancy is still possible until menopause is confirmed. Contraception is recommended until 12 consecutive months without a period if age ≥50, or 24 consecutive months if younger. Some methods also help manage heavy bleeding or other symptoms.

Cortisol
Cortisol is a hormone released by the adrenal glands in response to stress and low blood glucose. It helps regulate energy, metabolism, inflammation, and the sleep-wake cycle. Persistently elevated cortisol can worsen anxiety, sleep disruption, and weight changes during perimenopause.
Cortisol Awakening Response
The cortisol awakening response (CAR) is the natural spike in cortisol that occurs within the first hour after waking. It helps promote alertness and energy. Disruption of the CAR has been linked to chronic fatigue and stress dysregulation, which can be exacerbated during perimenopause.
Cytochrome P450 (CYP) Enzymes
CYP enzymes are proteins in the liver that metabolize many drugs, hormones, and supplements. Variations in CYP activity influence how substances are processed. Some botanical compounds and cannabidiol (CBD) can alter CYP activity, affecting drug levels and effects. Review supplement use with a clinician or pharmacist.
Depression
Depression is a mood disorder characterized by persistent sadness, lack of interest, and impaired functioning. During perimenopause, fluctuating hormones, sleep disruption, and stress may increase vulnerability. Treatment often includes therapy, lifestyle changes, and sometimes medication; professional evaluation is important when symptoms persist.
DEXA / Bone Density Test
A DEXA / Bone Density Test measures bone density to detect osteoporosis risk — typically recommended for women 65 + or younger with risk factors. It’s painless, quick, and helps determine fracture risk and need for preventive steps like calcium, vitamin D, or medication.
Dyspareunia
Dyspareunia means pain during sexual intercourse. In midlife, this symptom is often linked to genitourinary syndrome of menopause (GSM), where low estrogen leads to tissue thinning and dryness. Treatments include lubricants, vaginal moisturizers, pelvic floor therapy, or local estrogen therapy when appropriate.
Early Menopause
Menopause before age 45 is considered early menopause and may raise bone and heart risks. It can occur naturally or after medical treatments such as chemotherapy. Early recognition allows timely hormone evaluation and lifestyle measures to protect long-term health.

Endocannabinoid System (ECS)
The endocannabinoid system is a network of cellular receptors and signaling molecules that helps regulate sleep, mood, stress response, appetite, and pain perception. Cannabinoids such as CBD interact with this system, which is why research is exploring their potential role in sleep and stress support during perimenopause.

Endocrine System
The endocrine system is the collection of glands that produce and release hormones into the bloodstream. These hormones regulate growth, metabolism, reproduction, stress response, and sleep. Perimenopause reflects a major shift in endocrine function as ovarian hormone production becomes irregular and then declines.
Endometrial Hyperplasia
Endometrial hyperplasia is the thickening of the uterine lining caused by prolonged estrogen stimulation without adequate progesterone. It can cause abnormal bleeding and, if untreated, increase the risk of endometrial cancer. Management may involve progesterone therapy or surgical evaluation.
Estradiol Testing
Estradiol testing measures the most potent form of estrogen in the body. Because levels fluctuate widely during perimenopause, a single test cannot reliably confirm stage of transition, but serial testing may guide hormone therapy decisions or evaluate symptoms.
Estrogen (Estradiol, Estrone, Estriol)
Estrogen refers to a group of hormones that regulate reproductive function, bone density, cardiovascular health, brain signaling, and vaginal tissue. Estradiol is the dominant form during reproductive years; estrone becomes more prominent after menopause. Decline and fluctuation of estrogen drive many perimenopause symptoms.
Estrogen Dominance
Estrogen dominance describes a condition where the effects of estrogen outweigh the effects of progesterone. It is not an official medical diagnosis, but the term is used in some clinical contexts to explain symptoms like heavy bleeding, breast tenderness, or bloating. Interpretation requires clinical evaluation and testing.
Fatigue
Menopause fatigue is a persistent feeling of physical and mental tiredness that is not fully relieved by rest. In perimenopause, fatigue may result from disrupted sleep, fluctuating hormones, stress responses, and metabolic changes. It can affect concentration, mood, and daily functioning.
Final Menstrual Period (FMP)
The final menstrual period is the last natural menstrual bleed before menopause is confirmed. A woman is considered in menopause after 12 consecutive months without a period following the FMP.
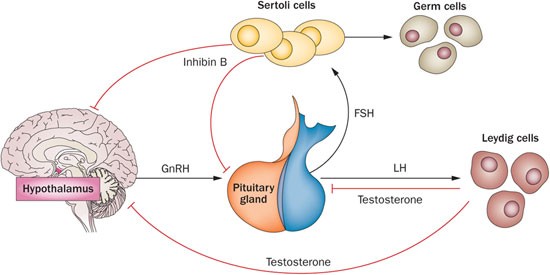
Follicle-Stimulating Hormone (FSH)
Follicle-Stimulating Hormone (FSH) is a hormone produced by the pituitary gland that stimulates the growth of ovarian follicles. As ovarian function declines in perimenopause, FSH levels rise in a compensatory manner. Because levels vary from day to day, a single FSH measurement cannot diagnose menopause.
Genitourinary Syndrome of Menopause (GSM) / Vulvovaginal Atrophy
Genitourinary syndrome of menopause means changes in the vaginal and urinary tissues caused by declining estrogen. It includes vaginal dryness, irritation, burning, discomfort during sex, and urinary urgency or recurrent infections. GSM tends to progress over time without treatment, but vaginal moisturizers, lubricants, pelvic floor therapy, and local estrogen can provide relief.
Gut Microbiome / Gut Microbiota
The gut microbiome is the community of bacteria and other microorganisms living in the digestive tract. It plays an important role in digestion, immune function, metabolism, and inflammation. Research shows that menopause is associated with shifts in gut microbiome diversity, which may influence weight regulation, metabolic health, and inflammatory symptoms in midlife.
Hormone
A hormone is a chemical messenger released by glands that travels through the bloodstream to instruct organs and tissues how to function. Hormones regulate metabolism, growth, reproduction, mood, and sleep. During perimenopause, hormone signaling becomes irregular, affecting multiple body systems at once.
Hormone Deficiency
Hormone deficiency occurs when the body produces lower-than-needed levels of a hormone. In menopause, estrogen and progesterone deficiency contribute to bone loss, cardiovascular changes, vaginal tissue thinning, and sleep disruption. Hormone therapy may be used when benefits outweigh risks.
Hormonal Fluctuation
Perimenopause is marked by fluctuating levels of estrogen, progesterone, and FSH, causing common symptoms. These hormonal fluctuations can trigger irregular cycles, hot flashes, night sweats, and sleep disturbance.
Hormonal Imbalance
Hormonal imbalance refers to disrupted hormone signaling patterns rather than a single abnormal lab value. During perimenopause, estrogen and progesterone can rise and fall unpredictably, leading to irregular cycles and fluctuating symptoms such as hot flashes, mood changes, and sleep disruption.
Hormone Receptor
A hormone receptor is a protein on or inside cells that receives hormone signals and triggers a response in that tissue. Estrogen and progesterone receptors exist in the brain, bones, heart, breasts, and reproductive organs. Changing hormone levels during perimenopause alter receptor activity, which is why symptoms affect many body systems.
Hormone Replacement Therapy (HRT) / Menopausal Hormone Therapy (MHT)
Hormone replacement therapy uses estrogen with or without progesterone to relieve menopause symptoms and protect bone health. It can be delivered through pills, patches, gels, sprays, or vaginal preparations. Treatment decisions are based on symptom severity, age, time since menopause, and personal health history.

Hot Flashes / Vasomotor Symptoms
Hot flashes are sudden waves of heat, flushing, and sweating caused by changes in the brain’s temperature-regulating center as estrogen levels decline. Night sweats are hot flashes that occur during sleep. These symptoms are common in perimenopause and can disrupt sleep and daily comfort.
Hysterectomy
A hysterectomy is surgery to remove the uterus. If the ovaries remain, hormone production may continue, but periods stop. If the ovaries are also removed, menopause occurs immediately and symptoms may be more intense due to sudden hormone loss.
Hypothalamic–Pituitary–Adrenal (HPA) Axis
The Hypothalamic–Pituitary–Adrenal Axis is the communication system between the brain and adrenal glands that controls the stress response through cortisol release. During perimenopause, ovarian hormone changes can influence HPA-axis sensitivity, contributing to anxiety, sleep disruption, and stress intolerance.
Hypothalamic–Pituitary–Ovarian (HPO) Axis
The Hypothalamic–Pituitary–Ovarian (HPO) Axis is the hormone feedback loop between the brain and ovaries that controls ovulation and menstrual cycles. During perimenopause, this system becomes less predictable, causing irregular periods and fluctuating hormone levels.
Insomnia
Insomnia is difficulty falling asleep, staying asleep, or waking too early, even when there is enough time for sleep. It is one of the most common perimenopause symptoms and is often driven by night sweats, stress activation, and circadian rhythm disruption.

Joint Pain
Joint pain refers to aching, stiffness, or soreness in the joints. During perimenopause and after menopause, lower estrogen levels may contribute to increased joint discomfort and stiffness, particularly in the morning. Regular movement, strength training, and medical evaluation can help manage symptoms.
Libido / Sexual Function
Libido refers to sexual desire and interest in intimacy. During perimenopause, libido can change due to hormonal shifts, fatigue, stress, and vaginal dryness. Addressing sleep, comfort, emotional connection, and medical options can improve sexual wellbeing.
Luteinizing Hormone (LH)
Luteinizing Hormone (LH) is a hormone released by the pituitary gland that triggers ovulation. After menopause, LH levels remain elevated because the ovaries no longer respond to stimulation.
Medical Menopause
Medical menopause occurs when medications suppress ovarian function, often during cancer treatment or for specific gynecological conditions. Hormone levels fall quickly, and symptoms can resemble sudden menopause.
Melatonin
Melatonin is a hormone produced by the brain that signals the body clock that it is time for sleep. It rises in the evening in response to darkness and falls in the morning with light. Melatonin supplements can help shift sleep timing for circadian rhythm disruptions, but they do not address all causes of perimenopausal insomnia or night waking.
Menopause
Menopause is diagnosed after 12 consecutive months without a menstrual period. It marks the end of natural fertility and the beginning of long-term estrogen and progesterone deficiency.
Menorrhagia
Menorrhagia means unusually heavy or prolonged menstrual bleeding. In perimenopause, irregular ovulation and hormone fluctuations can lead to heavier cycles. Persistent heavy bleeding should be evaluated to rule out underlying conditions.
Metabolic Syndrome / Insulin Resistance
Metabolic syndrome is a cluster of conditions including increased abdominal fat, high blood sugar, and abnormal cholesterol levels. After menopause, hormonal changes increase the risk of insulin resistance and weight gain.
Natural Menopause
Natural menopause occurs without surgery or medical intervention. It is confirmed after 12 consecutive months without a period.

Night Sweats
Night sweats are hot flashes that occur during sleep. They can disrupt rest, cause frequent awakenings, and contribute to chronic fatigue.
Non-Hormonal Therapies
Non-hormonal therapies include medications such as selective serotonin reuptake inhibitors (SSRIs), selective norepinephrine reuptake inhibitors (SNRIs), gabapentin, and clonidine. These may reduce hot flashes when hormone therapy is not appropriate.
Oophorectomy
An oophorectomy is surgery to remove one or both ovaries. When both ovaries are removed, menopause occurs immediately because estrogen and progesterone production stops.
Osteopenia
Osteopenia means lower-than-average bone density that has not yet reached the level of osteoporosis. It is a warning stage that indicates increased fracture risk if bone loss continues.
Osteoporosis
Osteoporosis is a condition in which bones become weak and fragile due to reduced density. After menopause, lower estrogen accelerates bone loss, increasing fracture risk in the spine, hips, and wrists.
Perimenopause
Perimenopause is the transitional stage before menopause when ovarian hormone production becomes unpredictable. It typically begins in the 40s and causes irregular cycles and early menopause symptoms.
:max_bytes(150000):strip_icc()/GettyImages-1199153914-18796a3613004eeb883113af6b4df36f.jpg)
Phytoestrogens
Phytoestrogens are plant compounds that weakly mimic estrogen in the body. They are found in foods like soy and flax and may modestly reduce hot flashes in some women.
Postmenopause
Postmenopause refers to the years after menopause has been confirmed. Hormone levels remain low and stable, making bone, heart, and cognitive health key priorities.
Premature Ovarian Insufficiency (POI)
Premature Ovarian Insufficiency (POI) occurs when ovarian function stops before age 40. It causes early estrogen deficiency and increases risks to bone and heart health without medical management.
Premenopause
Premenopause refers to the reproductive years before perimenopause begins, when cycles are still regular and ovarian hormone production is stable.
Premenstrual Syndrome (PMS)
PMS refers to physical and emotional symptoms that occur in the days before a period, such as bloating, irritability, and breast tenderness. Some women notice PMS patterns change during early perimenopause.
Premenstrual Dysphoric Disorder (PMDD)
Premenstrual Dysphoric Disorder (PMDD) is a severe form of PMS that significantly affects mood and daily functioning. Hormonal sensitivity plays a role, and symptoms can overlap with perimenopause-related mood changes.
Progesterone
Progesterone is a hormone produced after ovulation that balances estrogen, regulates menstrual cycles, and supports sleep and mood. It often declines early in perimenopause, contributing to irregular periods and insomnia.

Restorative Sleep
Restorative sleep is uninterrupted sleep that allows physical repair, memory processing, and emotional regulation. Perimenopause often disrupts restorative sleep through night sweats and nervous system activation.
Selective Estrogen Receptor Degrader (SERD)
Selective Estrogen Receptor Degrader (SERD) blocks and degrades estrogen receptors, mainly used in breast cancer treatment. They’re not typical menopause therapies but illustrate how hormonal pathways are targeted medically.
Selective Estrogen Receptor Modulator (SERM)
Selective Estrogen Receptor Modulator (SERM) acts like estrogen in some tissues (e.g., bone) and block it in others (e.g., breast). They are often prescribed to prevent osteoporosis or reduce breast cancer risk after menopause.
Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective Serotonin Reuptake Inhibitors (SSRIs) are medications that increase serotonin in the brain. They are sometimes prescribed to reduce hot flashes and support mood when hormone therapy is not suitable.
Selective Serotonin–Norepinephrine Reuptake Inhibitors (SNRIs)
Selective Serotonin–Norepinephrine Reuptake Inhibitors (SNRIs) affect serotonin and norepinephrine and may help reduce vasomotor symptoms and support mood stability.
Sleep Fragmentation
Sleep fragmentation refers to repeated nighttime awakenings that prevent continuous sleep cycles. It reduces sleep quality even when total sleep time appears adequate.

Sleep Hygiene
Sleep hygiene describes daily habits and environmental choices that support healthy sleep, such as consistent bedtimes, limited late caffeine or alcohol, and a cool, dark bedroom. Good sleep hygiene supports but does not replace medical treatment for persistent insomnia.
Sleep Latency
Sleep latency is the amount of time it takes to fall asleep after going to bed. Longer sleep latency is common in perimenopause due to stress and circadian rhythm sensitivity.
Surgical Menopause
Surgical menopause occurs when both ovaries are removed. Estrogen and progesterone levels drop suddenly, often causing more intense symptoms than natural menopause.
Thermoregulation
Thermoregulation is the body’s system for maintaining a stable internal temperature. Hormonal changes during perimenopause can disrupt this system, leading to hot flashes and night sweats.

Thyroid Disorders
Thyroid disorders involve over- or under-production of thyroid hormones. Because thyroid symptoms can mimic perimenopause, testing is often recommended when fatigue, weight change, or mood symptoms appear.
Urinary Incontinence
Urinary incontinence is the unintentional leakage of urine. It may result from pelvic floor changes and low estrogen effects on urinary tissues in midlife. Pelvic floor therapy and medical treatments can help.
Urinary Tract Infections (UTIs)
Urinary tract infections are bacterial infections of the bladder or urinary system. After menopause, tissue changes from lower estrogen can increase UTI risk in some women.
Vaginal Atrophy / Endometrial Atrophy
Vaginal atrophy occurs when low estrogen thins the uterine lining, changing bleeding patterns or causing pelvic discomfort. Burning, itching, spotting and pain with sex are common symptoms, as are frequent urination and urinary tract infections. Localized estrogen therapy may help relieve symptoms in postmenopausal women.
Vaginal Dryness
Vaginal dryness occurs when estrogen levels decline and vaginal tissues become thinner and less lubricated. It can cause irritation and pain during sex.
Vasodilation / Vasoconstriction
Vasodilation is the widening of blood vessels, while vasoconstriction is narrowing. Hormonal changes in perimenopause influence these processes and contribute to hot flashes.

Women’s Health Initiative (WHI)
The Women’s Health Initiative was a large U.S. research program that studied hormone therapy and other health factors in postmenopausal women. Its findings changed menopause care guidelines and continue to inform clinical decision-making today.
Shop Now
-

Best Sellers
Our Best Sellers collection features the most trusted and highly effective solutions...
-

Merchandise
Let the world know you're Perimenoproud with our high-quality merch! The perfect...
-

CBD Products
Perimenopause can be tough on your body. You may find it harder...
FAQs About Perimenopause
What is the difference between perimenopause and menopause?
Perimenopause is the stage before menopause when hormone levels fluctuate and periods become irregular. Menopause is confirmed after you have not had a period for 12 months in a row. Perimenopause often lasts for several years before menopause is official.
At what age does perimenopause usually begin?
Perimenopause usually starts in the mid-40s, but it can begin earlier or later. Your genes, smoking, and some health conditions can affect when it starts.
Why do hormone levels fluctuate during perimenopause?
As the ovaries slow down, the brain and ovaries send mixed signals about hormones. Estrogen and progesterone can go up and down in unpredictable ways, so symptoms may change from month to month.
What are the most common perimenopause symptoms?
Common symptoms are irregular periods, hot flashes, night sweats, trouble sleeping, brain fog, mood swings, tiredness, and vaginal dryness. Every woman’s symptoms can be different.
Why does sleep get worse during perimenopause?
Hormone changes can affect how your brain controls body temperature, stress, and sleep cycles. Night sweats, anxiety, and a more active nervous system can all make it harder to get good sleep.
Can blood tests confirm perimenopause?
A single hormone test cannot reliably diagnose perimenopause because hormone levels change from day to day. Doctors usually look at your symptoms and changes in your periods to make a diagnosis.
What is the endocrine system’s role in menopause?
The endocrine system makes hormones that control things like reproduction, sleep, metabolism, and how you handle stress. During perimenopause, the body goes through big changes as the ovaries make less hormones.
What is hormone replacement therapy (HRT)?
HRT gives estrogen, sometimes with progesterone, to help with menopause symptoms and protect your bones. The treatment plan depends on your age, health history, and how severe your symptoms are.
Are there non-hormonal treatment options?
Yes. There are non-hormonal medicines, therapy for sleep problems, lifestyle changes, and other treatments that can help if hormone therapy is not right for you or if you prefer not to use it.
Why does bone density decrease after menopause?
Estrogen helps keep bones strong. After menopause, lower estrogen causes bones to lose strength faster, which raises the risk of osteopenia and osteoporosis over time.
Is brain fog permanent?
Brain fog during perimenopause is usually temporary and gets better as your sleep and hormones even out. If thinking problems last, it’s a good idea to talk to a doctor.
Can lifestyle changes help with perimenopause symptoms?
Yes. Staying active, keeping a regular sleep schedule, managing stress, eating a balanced diet, and cutting back on alcohol and smoking can help many women feel better.
When should I speak with a doctor?
If your symptoms make it hard to sleep, work, maintain relationships, or enjoy life, or if your bleeding is much heavier or more irregular than usual, you should talk to a doctor.







